With construction projects nearing completion and in design, Columbus,Ohio, will see a major shift toward private hospital rooms in the next year. The provision of privacy and space creates an enhanced healing environment with higher patient satisfaction and better clinical outcomes
New, private rooms are often created through renovation rather than new construction. There are two major considerations for the backfill and renovation of these units: planning and design goals, and constructability. Let’s take a closer look at both.
1. Planning & Design
The facility’s overall system must be understood relative to the total number of inpatient rooms needed. In most cases, the creation of new, private rooms will not work within the existing room module so there could be a decrease in total beds with the renovation. The organization needs to ask themselves several key questions:
- What is the acceptable total number of beds for the facility when weighed against organic and strategic growth projections?
- Are the newly renovated beds to be used for medical-surgical, ICU level of care, or something in between?
- Does the facility have the flexibility to reconfigure and/or expand space to increase square footage of the inpatient room?
- What ratio of support area to inpatient bed area is the facility targeting?
Addressing these questions is critical to ensure that the renovation fulfills the needs of the facility. DesignGroup worked with a confidential client on a project that exemplifies the importance of these considerations. The hospital recently completed a new, inpatient tower and our goal was to renovate an existing unit for infectious disease while making it comparable to the new tower. The concepts of equivalency and excellence of patient care were paramount. The existing space was to be repurposed for a different patient population that required fewer beds; therefore larger, private rooms could be created while still achieving the target number. Also, there was adequate space in the core area of the floor which allowed for the rooms to be expanded toward the corridor, rather than increasing the size along the perimeter windows, which would reduce the potential total number of beds. In this example, due to the repurposing of the unit and availability of space, we were able to meet the client’s target size and number of beds, creating right sized rooms with right sized support spaces. If this approach is not feasible for your project, other options can be investigated.
2. Constructability
Parallel to tackling these planning and design considerations, the team focuses on the constructability of the renovation project. Items to address include:
- The number of units and floors being affected
- Infrastructure upgrades that will be required to support new technologies as units come online
- The number of beds that can be taken out of service at one time to accomplish the renovation
Careful study will need to be done in order to fully understand the ebb and flow of bed availability while renovation occurs. Dependent upon the overall scope, the team may want to consider renovating units by floor (horizontally), or by wing (vertically). There are trade-offs for both. Renovating vertically creates advantages for the MEP systems as the primary supply and return typically run vertically in a building, and top-down renovation is generally preferred for plumbing requirements. However, this may disrupt multiple patient populations within the facility. Alternatively, renovating an entire floor horizontally may make more sense functionally, but would require repeated work on the system’s infrastructure as work moves up or down through the building. The previously mentioned renovation focused on one floor, therefore it did not involve this type of analysis. However, careful coordination occurred to align design and construction sequencing with this project and a unit renovation on the floor immediately below. The following diagram was developed for another client who required comparison of vertical vs. horizontal phasing for a multi-floor renovation: 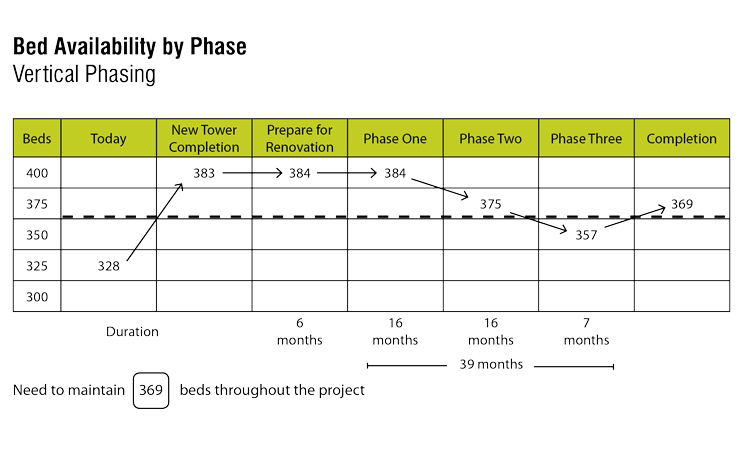
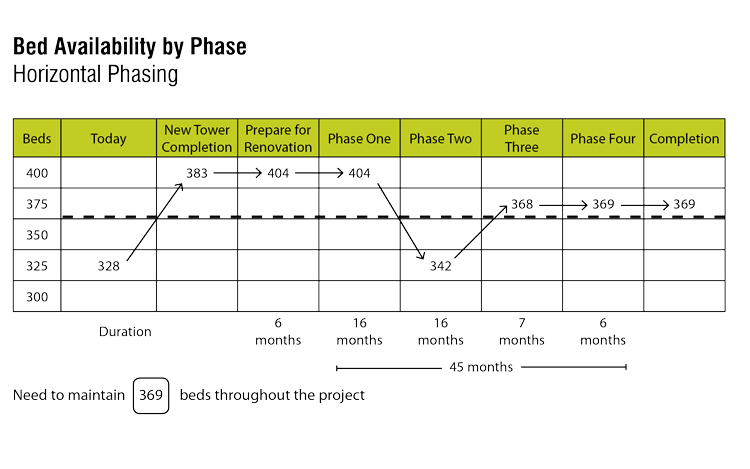 This particular study shows the number of beds that can be maintained through multiple phases remains higher and more consistent with vertical phasing than with horizontal phasing. Additionally, the horizontal phasing option requires a significantly lower drop in the number of beds for a longer period of time, 342 beds for 16 months, whereas in vertical phasing, the number of beds drops down to 357 for only seven months. The horizontal approach also encompasses a longer overall period of construction. Renovating inpatient units to larger, private rooms requires a great deal of consideration that includes a balance of quality versus quantity of space and an evaluation of the number of beds needed to maintain a viable operation. It is truly a team effort between the construction manager, architect, and owner to clarify objectives and achieve the goal of creating a better healthcare environment in which to give and receive the best level of care for patients.
This particular study shows the number of beds that can be maintained through multiple phases remains higher and more consistent with vertical phasing than with horizontal phasing. Additionally, the horizontal phasing option requires a significantly lower drop in the number of beds for a longer period of time, 342 beds for 16 months, whereas in vertical phasing, the number of beds drops down to 357 for only seven months. The horizontal approach also encompasses a longer overall period of construction. Renovating inpatient units to larger, private rooms requires a great deal of consideration that includes a balance of quality versus quantity of space and an evaluation of the number of beds needed to maintain a viable operation. It is truly a team effort between the construction manager, architect, and owner to clarify objectives and achieve the goal of creating a better healthcare environment in which to give and receive the best level of care for patients.
Jane Peters, AIA, ACHA, LEED AP BD+C, earned her Master of Architecture from Harvard University Graduate School of Design and has dedicated over 27 years to providing medical planning and architectural design services for healthcare organizations throughout the country.
